
Power Plants
Many of the most powerful drugs in modern medicine’s arsenal came from natural products, from penicillin to the chemotherapy agents Taxol® and vincristine.

Many of the most powerful drugs in modern medicine’s arsenal came from natural products, from penicillin to the chemotherapy agents Taxol® and vincristine.

What dietary behaviors may cut the odds of developing of an abdominal aortic aneurysm (AAA) in half?

A million Americans have a silent aneurysm in their abdominal aorta (AAA) that may become life-threatening over time.

Cardiologists suggest that cholesterol-lowering statin drugs be given out free with fast food meals

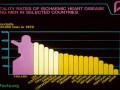
The average “bad” cholesterol (LDL) level in people having heart attacks is in the “near-optimal” range, suggesting that the current guidelines are too lax.

Most people hospitalized with heart attacks have cholesterol levels considered “desirable” under the current recommendations. Having a “normal” cholesterol in a society where it’s normal to die of heart disease is not necessarily a good thing.

Why the current vitamin D recommendations may be too low, other expert recommendations may be too high, and 2000 international units a day may be just right.

People respond differently to the same level of vitamin D supplementation, making it difficult to formulate one-size-fits-all guidelines.

To reach the circulating (25-hydroxy) vitamin D levels associated with the lowest overall mortality, one may need to take supplements, given data suggesting suboptimal production from sun—even under optimal circumstances.
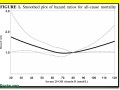
Vitamin D deficiency may shorten one’s lifespan, but getting too much vitamin D may also adversely affect longevity.

The Institute of Medicine’s conservative position on vitamin D is understandable, given the history of hyped vitamin supplements (vitamin A, beta carotene, folic acid, vitamin C, vitamin E) that turned out worthless—or worse.
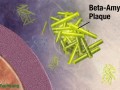
Ginger and apple juice appear to protect human nerve cells from the neurotoxic Alzheimer’s plaque protein amyloid beta in a petri dish.

The USDA Dietary Guidelines Committee stands accused of ignoring the science to justify its recommendation to eat meat.
The success story in Finland shows that science-based dietary guidelines can save millions of lives.
Why does the medical establishment sometimes ignore highly efficacious therapies, such as plant-based diets, for heart disease prevention and treatment?

The China-Oxford-Cornell Diet and Health Project directed by T. Colin Campbell and colleagues showed that chronic diseases, such as heart disease, are not inevitable consequences of aging.

Dr. Dean Ornish proved decades ago that heart disease could be reversed solely with diet and lifestyle changes.

Medicare is now accepting for reimbursement the Dean Ornish Program for Reversing Heart Disease and the Pritikin Program, which, on a personal note, is what inspired me to go into medicine.

In a double-blind study, the spice saffron beat out placebo in the treatment of Alzheimer’s disease dementia symptoms.

Los virus que causan verrugas en los animales podrían ser más que un problema cosmético para los consumidores

El mayor estudio prospectivo sobre nutrición nunca antes publicado sugiere que la grasa animal puede estar implicada en el desarrollo del cáncer de páncreas.

¿Qué tipo de alimentación basada en plantas es más efectiva en la reducción de los niveles de colesterol?

Pagar por una vida más corta.

Los beneficios del consumo de café.

¿Deben las mujeres con cáncer de mama con receptores de estrógeno positivos evitar los alimentos de soja?

El Estudio de Salud de Medicos de Harvard sugiere que aquellos que comen un huevo diario tienen vidas mas cortas.

Hay dos vitaminas que no son producidas por las plantas que pueden requerir suplementación.

Pagar para vivir menos.

Tres acciones que pueden reducir a la mitad el riesgo de muerte de nuestro asesino número uno.

Las maravillas de las bayas.

Los investigadores descubrieron una intervención dietética que puede ralentizar la progresión del cáncer.