Losing weight can reduce sciatica, hypertension, and cancer risk, as well as reverse type 2 diabetes.
In the ABCs of the health consequences of obesity, A is for Arthritis, as I discussed in my previous blog post, and B is for Back Pain. Being overweight is not just a risk factor for low back pain, but it is also a risk factor for sciatica (a radiating nerve pain), as well as degenerating lumbar discs and disc herniation. Similar to what we learned in the arthritis story, this may also be due to a combination of the excess weight, high cholesterol, and inflammation associated with being overweight. Why cholesterol? Studies of autopsies and angiographies show that the lumbar arteries that feed our spine can get clogged with atherosclerosis and starve the disks in our lower back, as you can see below and at 0:47 in my video The Effects of Obesity on Back Pain, Blood Pressure, Cancer, and Diabetes.

B is also for Blood Pressure. Excess visceral fat—for example, internal abdominal fat—can physically compress our kidneys. The increased pressure can effectively squeeze sodium back into our bloodstream, increasing our blood pressure. Together, the combination of obesity and hypertension can have “disastrous health implications,” but the good news is that just a few pounds of weight loss can help take off the pressure. Losing excess weight has been described as “a vital strategy for controlling hypertension.” In fact, researchers found that losing around nine pounds (4 kg) may lower blood pressure about as much as cutting salt intake approximately in half can.
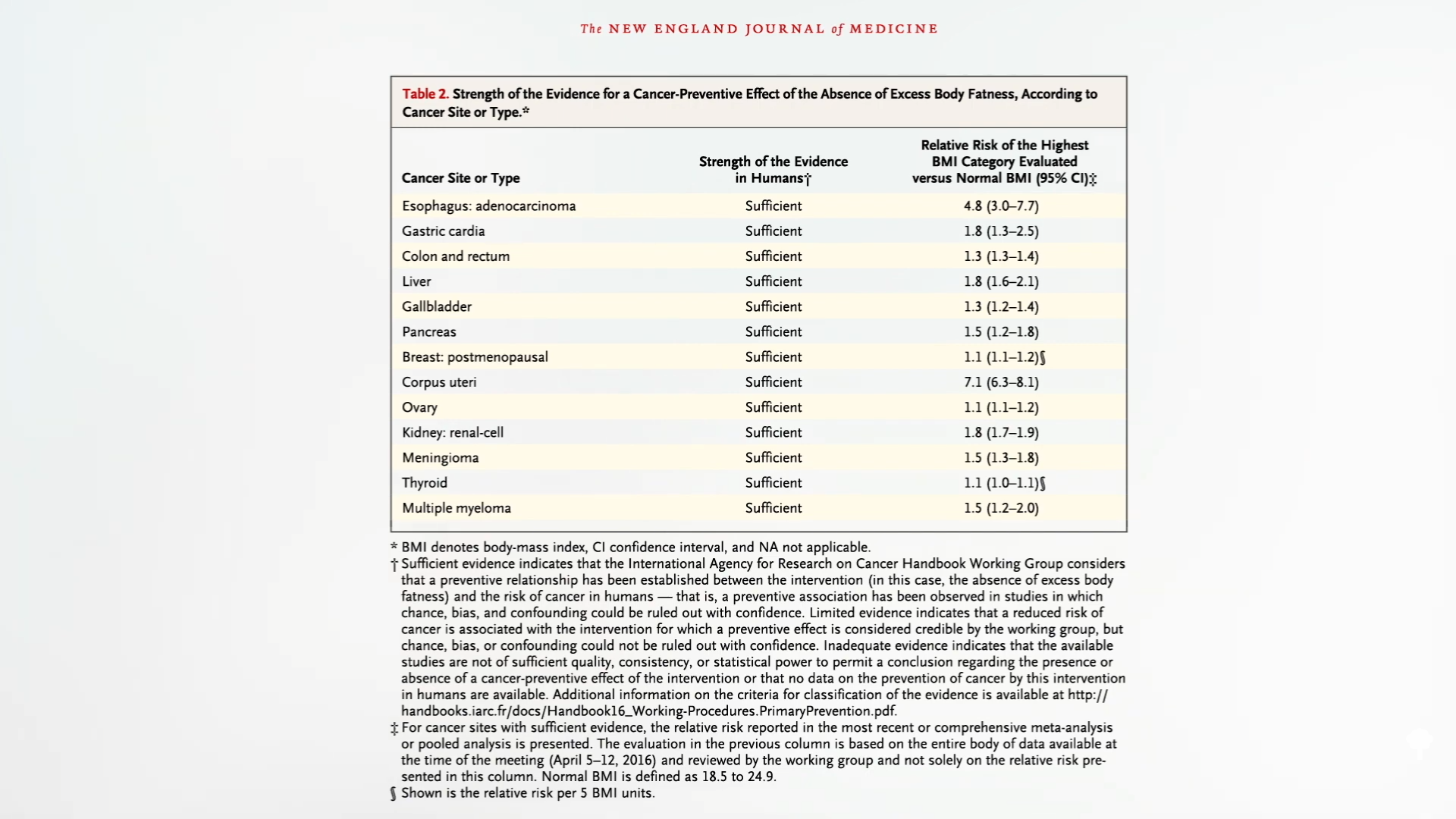
C is for Cancer. As many as three-quarters of people surveyed “were unaware that being overweight or obese increased a person’s risk of cancer,” when, in fact, based on a comprehensive review of more than a thousand studies, excess body fat raises the risk of most cancers, including esophageal, stomach, colorectal, liver, gallbladder, pancreatic, breast, uterine, ovarian, kidney, brain, thyroid, and bone marrow (multiple myeloma) cancers, as you can see below and at 2:00 in my video.
It could be the chronic inflammation of obesity or perhaps it is the high insulin levels due to insulin resistance. (Besides controlling blood sugars, insulin is also “a potent growth factor” that can promote tumor growth.) In women, it could also be the excess estrogen.
After the ovaries shut down at menopause, fat takes over as the principal site of estrogen production. That’s why women who are obese have up to nearly twice the estrogen levels circulating in their bloodstream, which is associated with an increased risk of developing breast cancer and dying from it. The data on prostate cancer aren’t as strong, though obesity is associated with increased risk of invasive penis cancer.
One of the reasons we’re confident the link between obesity and cancer is cause-and-effect—and not just an indirect consequence of eating poorly—is that the overall risk of cancer goes down when people lose weight, even through bariatric surgery. Researchers found that those experiencing a sustained weight loss of about 40 pounds (19.9 kg) after surgery went on to develop around one-third fewer cancers over the subsequent decade, compared with matched individuals in the nonsurgical control group who continued to slowly gain weight over time. The exception, though, is colorectal cancer.
“Colorectal cancer is the only known malignancy where the risk of being diagnosed with disease seems to increase after obesity surgery.” Indeed, after bariatric surgery, the rate of rectal cancer death may triple. The rearrangement of anatomy involved in one of the most common surgeries—Roux-en-Y gastric bypass—is thought to increase bile acid exposure along the intestinal lining. This causes sustained pro-inflammatory changes even years after the procedure, which is thought responsible for the increased cancer risk. In contrast, losing weight by dietary means has the potential to decrease obesity-related cancer risk across the board.
D is for Diabetes. As presented in a consensus statement from the International Diabetes Federation, obesity is considered the single most important risk factor for the development of type 2 diabetes, which is the leading cause of kidney failure, lower-limb amputations, and adult-onset blindness. Ironically, many of the leading drugs used to treat diabetes (including insulin itself) cause further weight gain, creating a vicious cycle.
So, again, using lifestyle medicine to treat the underlying cause is not only safer, simpler, and cheaper, but can also be most effective.
If you missed my previous video, check out The Best Knee Replacement Alternative for Osteoarthritis Treatment.
Coming up next? See related posts below.
I continue the topic of weight control with these videos that may be of interest to you: Is the Obesity Paradox Real or a Myth? and Friday Favorites: What’s the Ideal BMI and Waist Size?.
For more on back pain, blood pressure, cancer, and diabetes, check out their topic pages.
