What is the return on investment for educating employees about healthy eating and living?
“How do you wipe out the nation’s heart disease epidemic?” Those were the opening words to an editorial by Dr. Michael Jacobson, co-founder of Center for Science in the Public Interest, in the October 2005 issue of the charity’s Nutrition Action publication. Wrote Jacobson, “The best approach I’ve seen is the Coronary Health Improvement Project (CHIP),” which was renamed the Complete Health Improvement Program and then most recently, Pivio. CHIP tells people to eat more whole plant foods and less meat, dairy, eggs, and processed junk. It is considered to be “a premier lifestyle intervention targeting chronic disease that has been offered for more than 25 years.” More than 60,000 individuals have completed the program, which I discuss in my video A Workplace Wellness Program That Works.
Most CHIP classes are “facilitated by volunteer directors, sourced primarily through the Seventh-Day Adventist Church, who had an interest in positively influencing the health of their local community.” Why the Adventists? Their “health philosophy is built around the holistic biblical notion” that the human body should be treated as a temple. What’s more, many CHIP participants are Adventists, too. Is that why the program works so well? Because they have faith? You don’t know until you put it to the test.
Researchers looked at the influence of religious affiliation on responsiveness to CHIP, studying 7,000 participants. Even though Seventh-Day Adventists (SDAs) make up less than 1 percent of the U.S. population, about one in five CHIP-goers were Adventists. How did they do, compared with the non-Adventists (non-SDAs)? “Substantial reductions in selected risk factors were achieved…for both SDA and non-SDA,” but some of the reductions were greater among the non-Adventists. “This indicates that SDA do not have a monopoly on good health…”
Middle class, educated individuals also disproportionally make up CHIP classes. Would the program work as well in poverty-stricken populations? Researchers tried to reduce chronic disease risk factors among individuals living in rural Appalachia, one of the poorest parts of the country. “Conventional wisdom has been that each participant needs financial ‘skin in the game’ to ensure their attentiveness and commitment” to lifestyle change programs. So, if offered for free to impoverished communities, the results might not be as good. In this case, however, the “overall clinical changes in this pilot study [were] similar to those found in other 4-week CHIP classes throughout the United States,” suggesting CHIP may have benefits that “cross socioeconomic lines” and are “independent of payment source.” So, why don’t employers offer it free to employees to save on health care costs? CHIP is “described…as ‘achieving some of the most impressive clinical outcomes published in the literature,’” including “clinical benefits of the intervention, as well as its cost-effectiveness…”
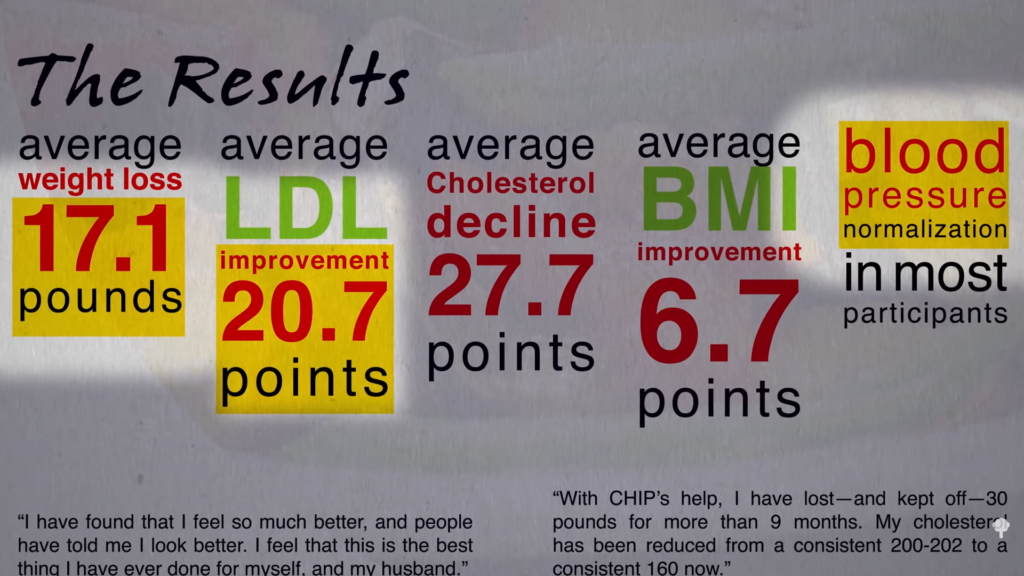
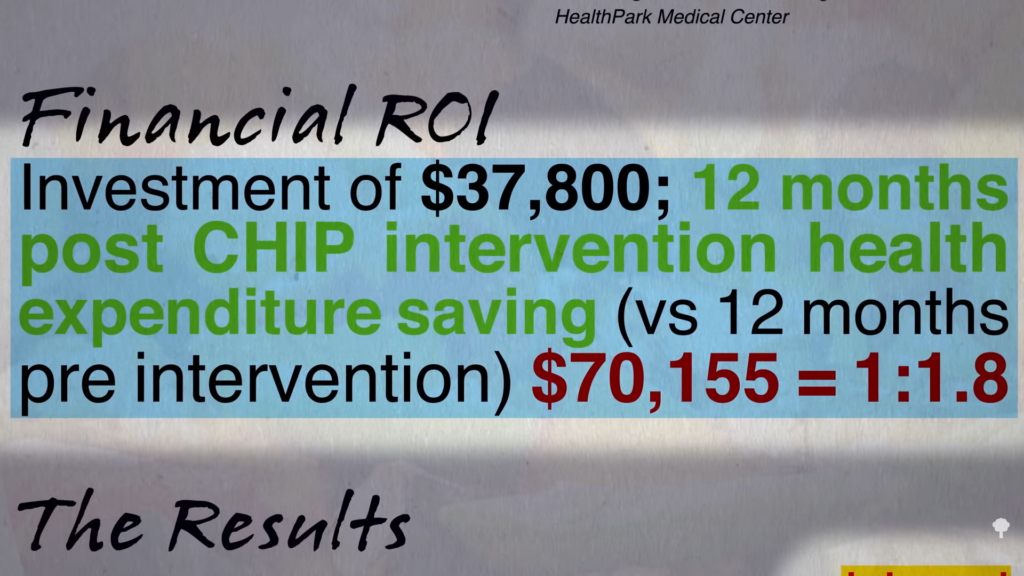
Lee Memorial, a health care network in Florida, offered CHIP to some of its employees as a pilot program. (Sadly, health care workers can be as unhealthy as everyone else.) As you can see below and at 3:05 in my video, they reported an average 17-pound weight loss, a 20-point drop in bad LDL cholesterol, and blood pressure normalization in most participants. Lee Memorial initially invested about $38,000 to make the program happen, but then saved $70,000 in reduced health care costs in just that next year. How? Because the employees became so much healthier. They got a financial return on investment of 1.8 times what they put in.
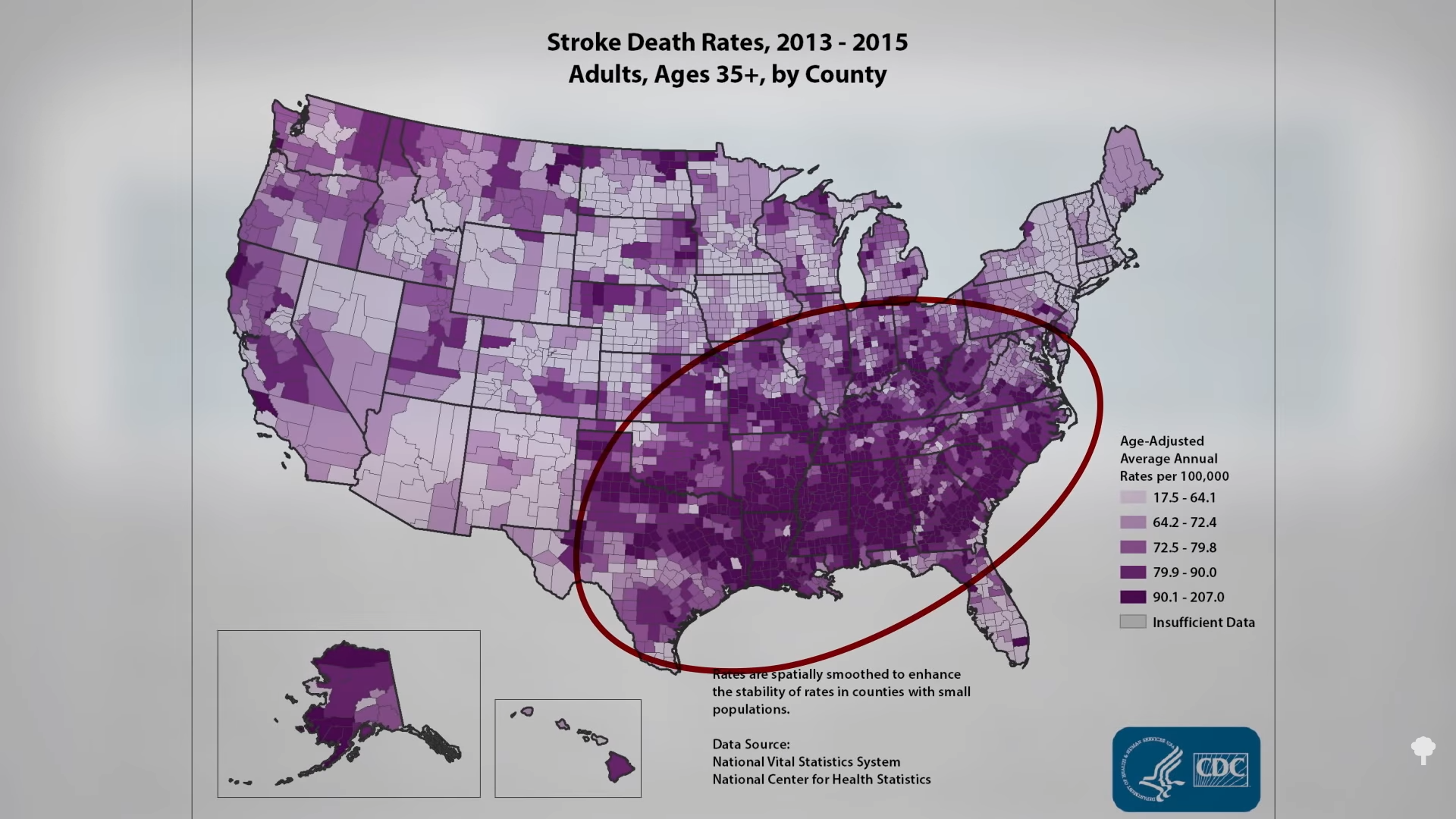
There hadn’t been a return on investment (ROI) study in the peer-reviewed medical literature until Dexter Shurney stepped up to the plate and published a workplace study out of Vanderbilt. “There was a high degree of skepticism at the planning stage of this study that active engagement could be realized in a sizable portion of the study group around a lifestyle program that had as its main tenets exercise and a plant-based diet.” Vanderbilt is, after all, in Tennessee, smack dab in the middle of the Stroke Belt, known for its Memphis ribs. (You can see a graphic of “Stroke Death Rates…by County” by the Centers for Disease Control and Prevention below and at 3:55 in my video.) Nevertheless, the subjects got on board enough to improve their blood sugar control and cholesterol. They also reported “positive changes in self-reported physical health and well-being. Health care costs were substantially reduced for study participants compared to the non-participant group.” For example, nearly a quarter of the participants were able to eliminate one or more of their medications, so they got about a two-to-one return on investment within just six months, providing evidence that just “educating a member population about the benefits of a plant-based, whole-foods diet is feasible and can reduce associated health care costs.”
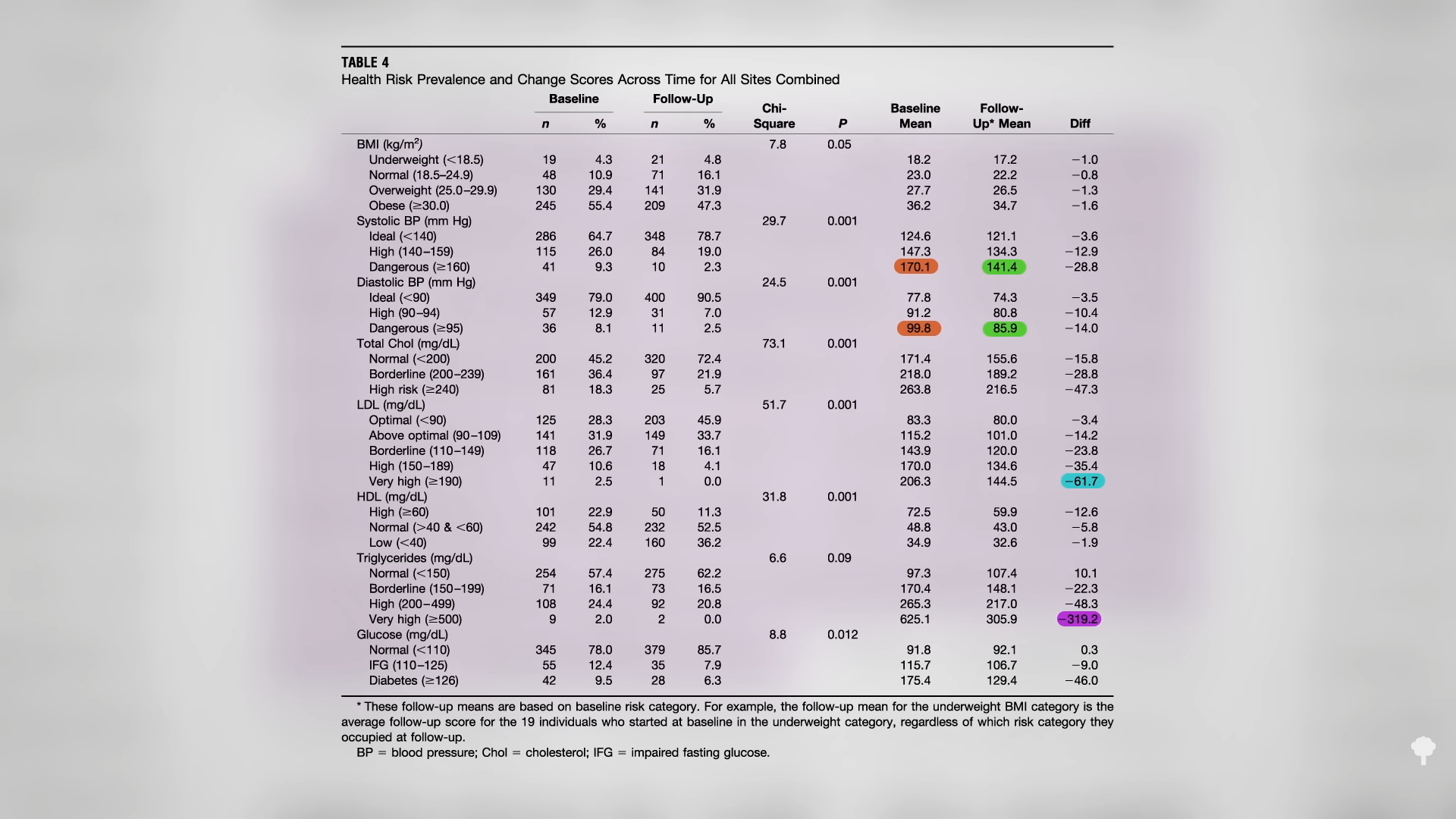
The largest workplace CHIP study done to date involved six employee populations, including, ironically, a drug company. The study included a mix of white-collar and blue-collar workers. As you can see below and at 4:40 in my video, there were dramatic changes experienced by the worst off. Those starting with blood pressures up around 170 over 100 saw their numbers fall to around 140 over 85. Those with the highest LDL cholesterol dropped 60 points and had a 300-point drop in triglycerides, as well as a 46-point drop in fasting blood sugars. Theoretically, someone coming into the program with both high blood pressure and high cholesterol might “experience a 64% to 96% reduction in overall risk of myocardial infarction,” a heart attack, our number one killer.
As Dr. Jacobson concluded in his editorial in Nutrition Action, “For the cost of a Humvee, any town could have a CHIP of its own. For the cost of a submarine or a farm subsidy, the entire country could get a CHIP on its shoulder.”
