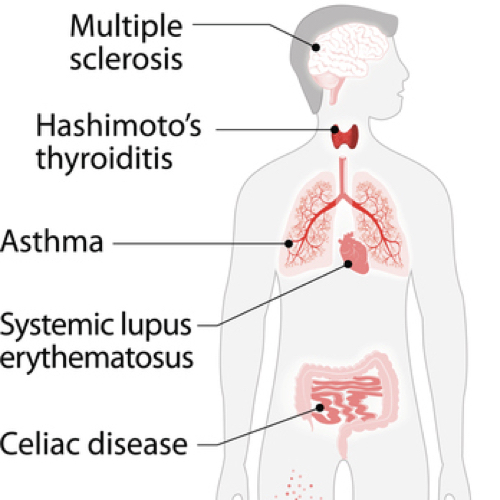
Autoimmune Diseases
A healthy immune system fights germs, budding cancers, and other harmful threats. Autoimmune diseases develop when our immune system mistakenly attacks our own healthy tissue. This may lead to inflammation and damage to joints, nerves, skin, tissues, muscles, and other organs.
Rheumatoid arthritis is a chronic, systemic autoimmune disease characterized by persistent pain and stiffness, along with progressive joint destruction, particularly in the hands and feet, leading to crippling deformities. How might we prevent and treat it?
In a famous 13-month-long randomized controlled trial of plant-based diets for rheumatoid arthritis, patients were put on a vegan diet for three and a half months, then switched to an egg-free lacto-vegetarian diet for the remainder of the study. Compared to the control group, who didn’t change their diet at all, the plant-based group had a significant improvement in morning stiffness within the first month, halving the number of hours they suffered joint stiffness. Pain dropped from five out of ten down to less than three out of ten. The plant-based group also reported subjectively feeling better and experiencing significant improvement in their grip strength, fewer tender joints, less tenderness per joint, and less swelling, with the added benefit of losing about 13 pounds. They also had a drop in inflammatory markers in their blood. Why? One way plant-based diets may help is by decreasing exposure to an inflammatory compound found in animal products.
Arthritis may also be triggered by Yersinia bacteria, which reportedly sickens nearly 100,000 Americans yearly. In every outbreak for which a source has been found, the culprit appears to be contaminated pork. Studies have found that within a year of contracting Yersinia food poisoning, victims appear 47 times more likely to come down with autoimmune arthritis, and the bacteria may also play a role in triggering an autoimmune thyroid condition known as Graves’ disease.
Not only may plant-based diets improve or even eliminate arthritis symptoms, but specific plant foods may provide some relief. For example, açai berries showed modest benefit for osteoarthritis sufferers. Tart cherries appear to be so anti-inflammatory that they can be used to treat a painful type of arthritis called gout. Delicious dietary treatments are much welcomed, as some gout drugs can cost $2,000 a dose, carry no clear-cut distinction between nontoxic, toxic, and lethal doses, or can cause a rare life-threatening side effect in which your skin detaches from your body.
For substantiation of any statements of fact from the peer-reviewed medical literature, please see the associated videos below.
Image Credit: ttsz / Thinkstock. This image has been modified.
Popular Videos for Autoimmune Diseases

Does Nutritional Yeast Trigger Crohn’s Disease?
Is the exaggerated reaction of many Crohn’s disease patients to baker’s, brewer’s, and nutritional yeast...
Sodium & Autoimmune Disease: Rubbing Salt in the Wound?
There are two ways in which salt may drive autoimmune diseases such as multiple sclerosis,...
How to Treat Asthma with a Low-Salt Diet
Cutting two teaspoons of salt’s worth of sodium from one’s daily diet can significantly improve...
Does Paratuberculosis in Meat Trigger Type 1 Diabetes?
The majority of specialists in the field agreed that paraTB in meat and dairy likely...
Does Paratuberculosis in Milk Trigger Type 1 Diabetes?
“Fear of consumer reaction” led the U.S. dairy industry to suppress the discovery in retail...
Meat Consumption and the Development of Type 1 Diabetes
Eating meat during breastfeeding is associated with an increased risk of type 1 diabetes, perhaps...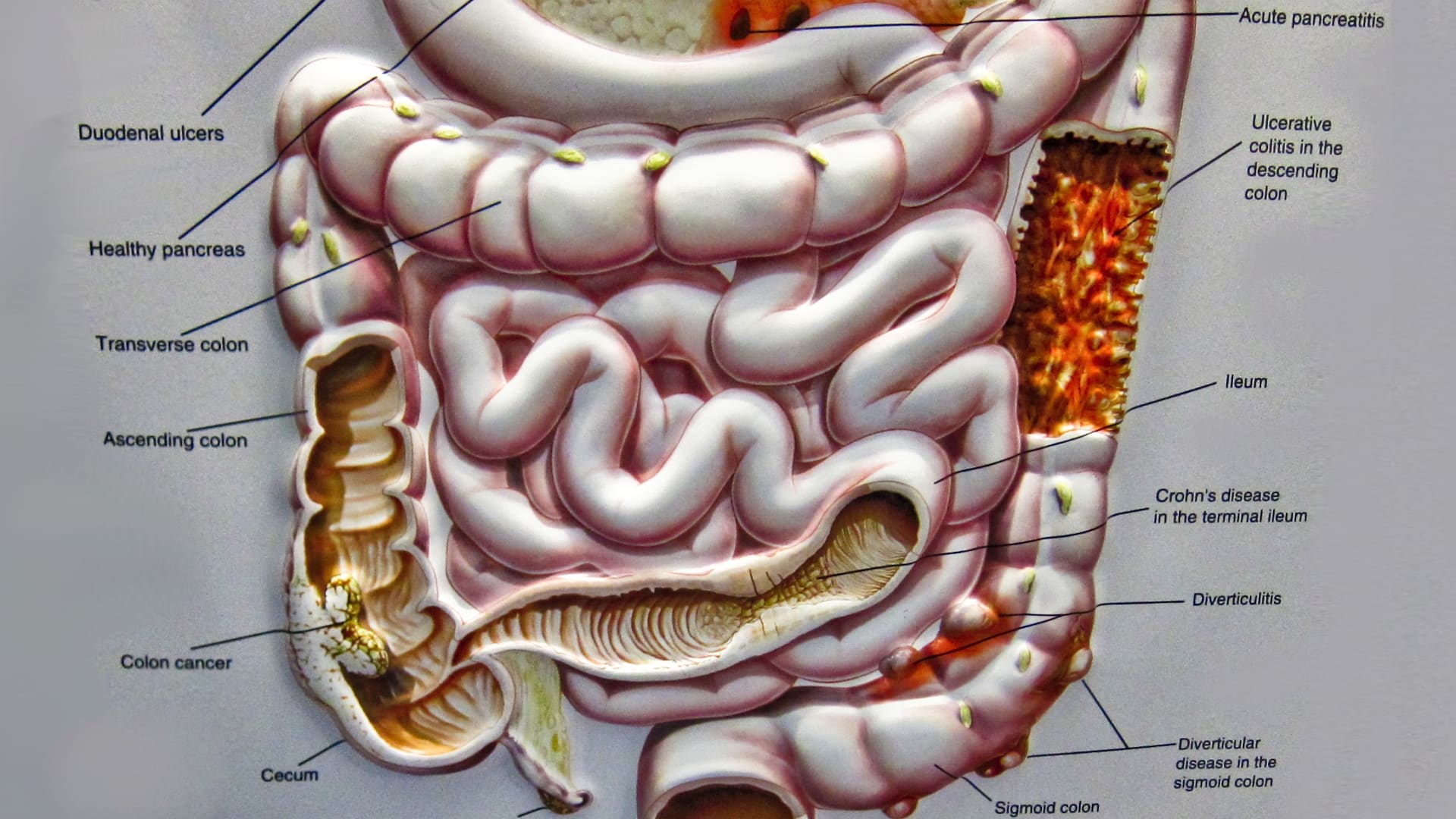
Preventing Crohn’s Disease with Diet
Diets centered around whole plant foods may help prevent Crohn’s disease through the benefits of...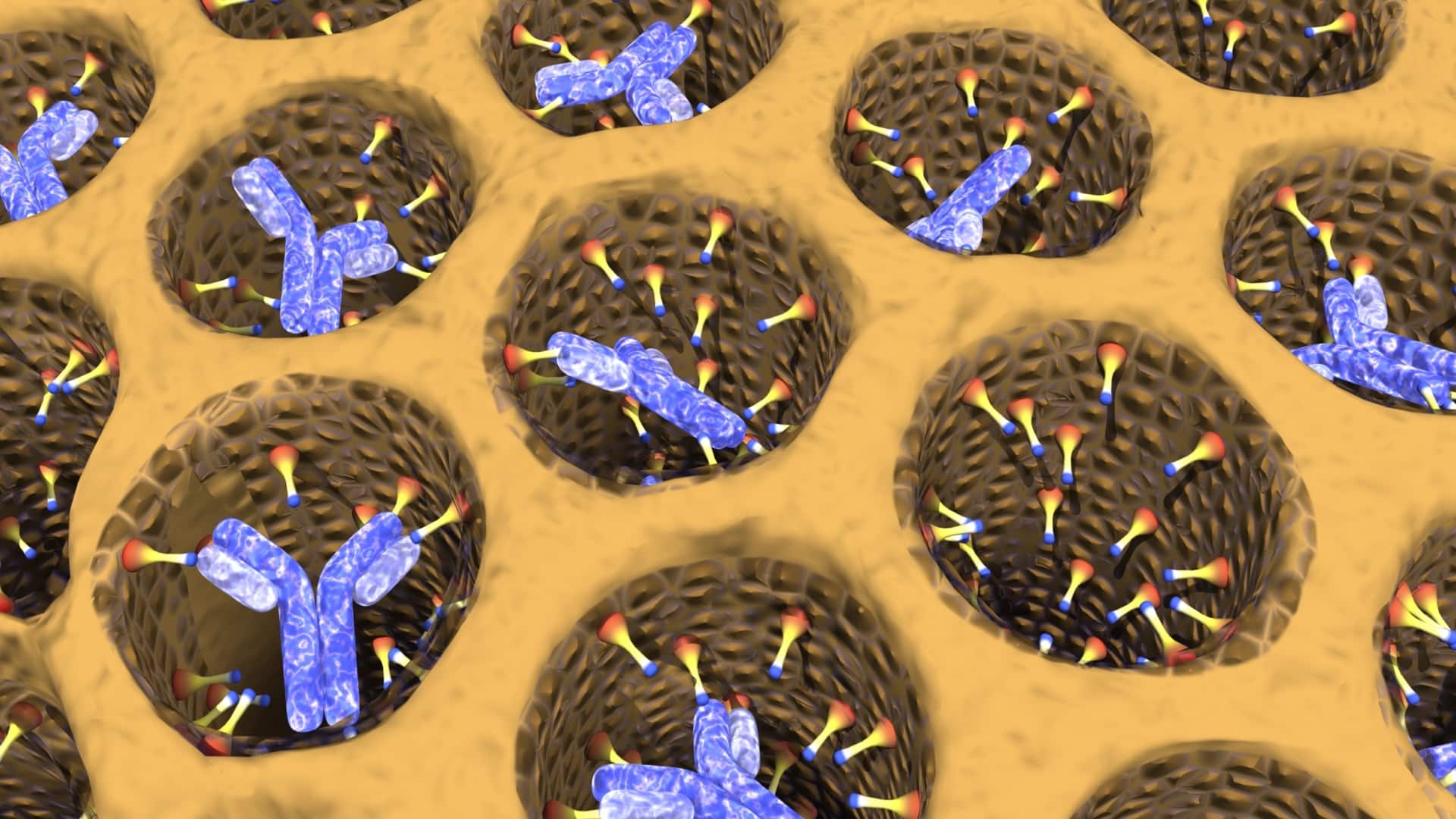
Why Do Plant-Based Diets Help Rheumatoid Arthritis?
Rheumatoid arthritis may be triggered by autoimmune friendly fire against a urinary tract infection bacteria...
Eczema Treatment with Coconut Oil, Mineral Oil vs. Vaseline
Natural topical remedies for eczema, including licorice root gel, St. John’s Wort cream, and emollients...
Treating Asthma and Eczema with Plant-Based Diets
Pilot studies on treating allergic eczema and severe asthma with dietary interventions have shown remarkable...All Videos for Autoimmune Diseases
-

Risks of NAD+ Boosting Supplements
Particular caution should be used for NAD+-boosting supplements by those with cancer, a personal or strong family history of cancer and perhaps also by those with inflammatory disorders and certain active infections.
-

The Best Way to Boost NAD+: Supplements vs. Diet (webinar recording)
The pros and cons of all the NAD+ supplements and what are the ways to boost NAD+ naturally with diet and lifestyle?
-

Fewer Than 1 in 5,000 Meet Sodium and Potassium Recommended Intakes
A staggering 99.99 percent of Americans fail to get the minimum recommended potassium intake (despite it being perhaps only half of our natural intake) and stay below the recommended sodium intake (even though it may be twice our natural intake).
-

How to Boost FGF21 with Diet for Longevity
Fasting and exercise can boost the longevity hormone FGF21, but what can we eat—or avoid eating—to get similar effects?
-

Diet for Hypothyroidism: A Natural Treatment for Hashimoto’s Disease
What were the results of a randomized, double-blind, placebo-controlled trial of a half teaspoon of powdered black cumin a day in Hashimoto’s (autoimmune thyroiditis) patients?
-

The Best Diet for Hypothyroidism and Hyperthyroidism
Is the apparent protection of plant-based diets for thyroid health due to the exclusion of animal foods, the benefits of plant foods, or both?
-

The Effects of Obesity on the Immune System and Kidney and Liver Diseases
What are the effects of weight loss on natural killer cell function, our first line of immune defense against cancer, as well as kidney function and fatty liver disease?
-

Fasting for Autoimmune Diseases
Various fasting regimens have been attempted for inflammatory autoimmune diseases such as lupus, ankylosing spondylitis, chronic urticaria, mixed connective-tissue disease, glomerulonephritis, and multiple sclerosis, as well as osteoarthritis and fibromyalgia.
-

Fasting for Rheumatoid Arthritis
Fasting, followed by a plant-based diet, is put to the test for autoimmune inflammatory joint disease.
-

Type 1 Diabetes Treatment: A Plant-Based Diet
Is it possible to reverse type 1 diabetes if caught early enough?
-

Anti-Inflammatory Diet for Lupus
Green smoothies are put to the test for the autoimmune disease SLE (lupus).
-

The World’s Largest Fasting Study
Buchinger modified fasting is put to the test.
-

Does Intermittent Fasting Increase Human Life Expectancy?
Alternate-day modified fasting is put to the test for lifespan extension.
-

Is Aloe Vera Gel the Best Treatment for Lichen Planus?
We shouldn’t ever swallow aloe vera, but how does using it topically for a chronic inflammatory autoimmune disease compare to steroids?
-

The Role of Dairy and Gluten in Canker Sores
Does excluding dairy products, food additives, and gluten-containing grains from one’s diet help those with recurring canker sores (aphthous ulcers)?
-

Eczema Treatment with Coconut Oil, Mineral Oil vs. Vaseline
Natural topical remedies for eczema, including licorice root gel, St. John’s Wort cream, and emollients such as coconut oil, mineral oil, and petroleum jelly, are put to the test.
-

Eczema Treatment with Evening Primrose Oil, Borage Oil vs. Hempseed Oil
Are there dietary supplements that can help with atopic dermatitis?
-

Dietary Cure for Hidradenitis Suppurativa
What is the role of dairy- and yeast-exclusion diets on arresting and reversing an inflammatory autoimmune disease?
-

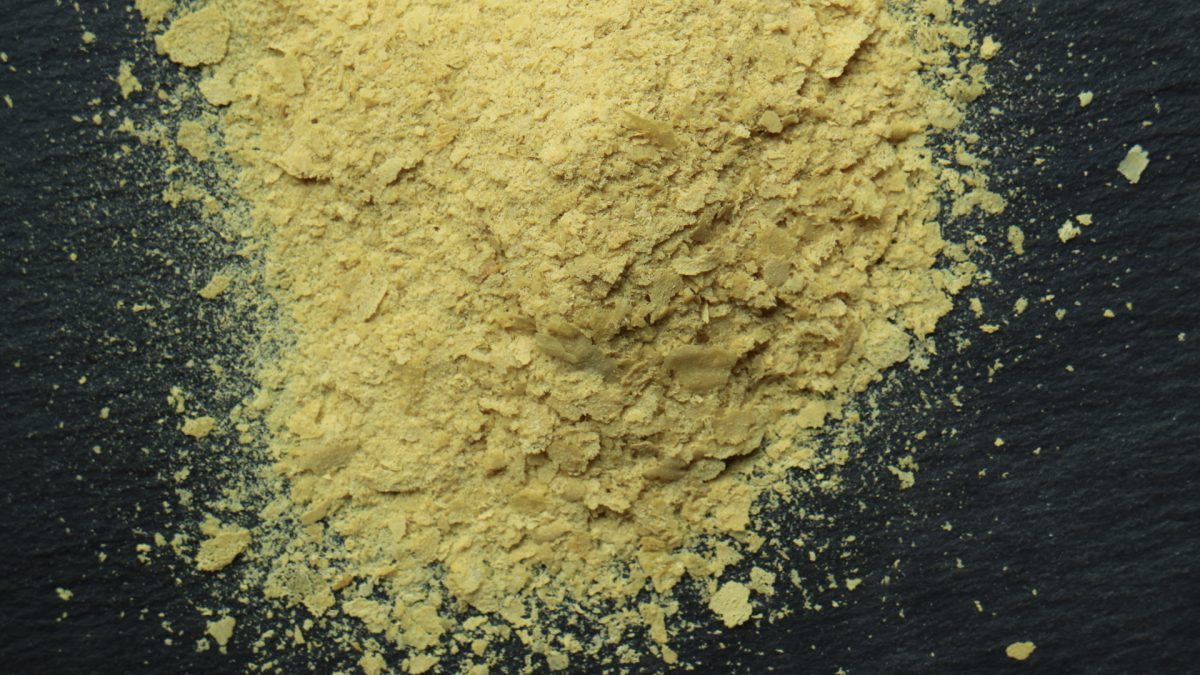
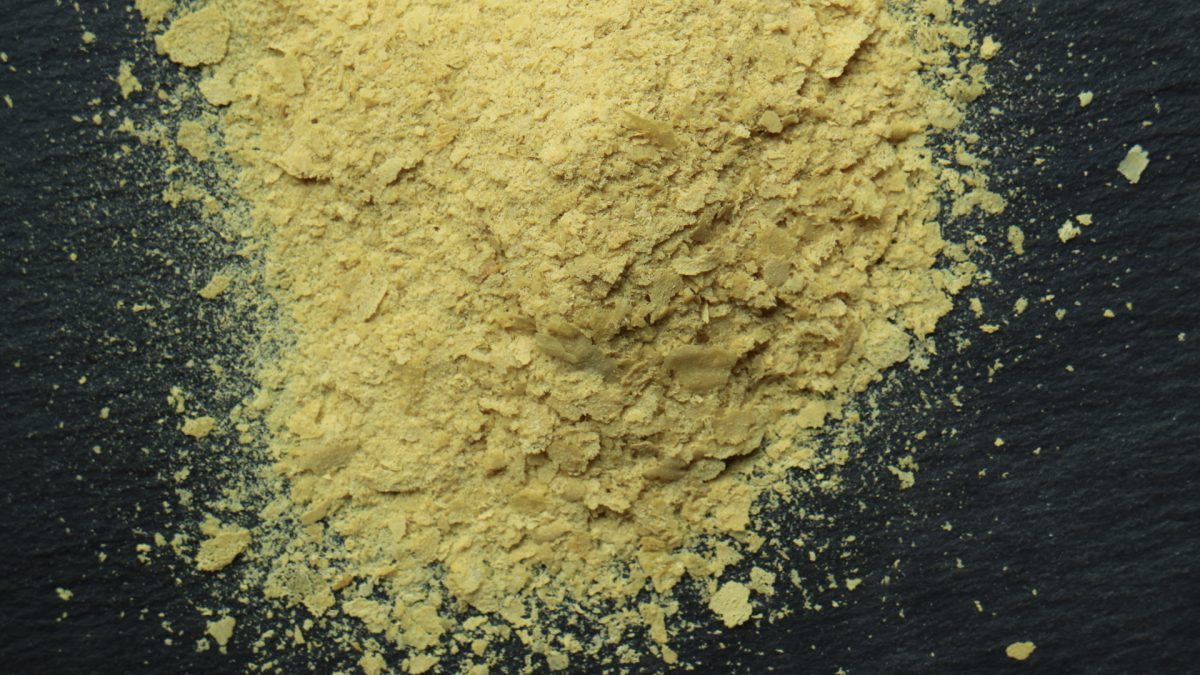
Is Nutritional Yeast Healthy for Everyone?
Those with certain autoimmune diseases such as Crohn’s disease should probably not eat nutritional yeast.
-
Is Candida Syndrome Real?
Does the presence of Candida in stool correlate with “Candida-hypersensitivity” symptoms, such as headaches and tiredness? And what happens when people are placed on a high-sugar diet?
-

Does Nutritional Yeast Trigger Crohn’s Disease?
Is the exaggerated reaction of many Crohn’s disease patients to baker’s, brewer’s, and nutritional yeast just a consequence of their inflamed leaky gut, or might the yeast be a contributing cause?
-

Sodium & Autoimmune Disease: Rubbing Salt in the Wound?
There are two ways in which salt may drive autoimmune diseases such as multiple sclerosis, psoriasis, type I diabetes, Sjögren’s syndrome, asthma, and rheumatoid arthritis.
-

How to Treat Asthma with a Low-Salt Diet
Cutting two teaspoons of salt’s worth of sodium from one’s daily diet can significantly improve lung function in asthmatics.
-

Does Paratuberculosis in Meat Trigger Type 1 Diabetes?
The majority of specialists in the field agreed that paraTB in meat and dairy likely represents a risk to human health and should be a high- or medium-priority public health issue.
-

Meat Consumption and the Development of Type 1 Diabetes
Eating meat during breastfeeding is associated with an increased risk of type 1 diabetes, perhaps a consequence of meat glycotoxins or paratuberculosis bacteria that may be passed though breast milk.
-

Does Paratuberculosis in Milk Trigger Type 1 Diabetes?
“Fear of consumer reaction” led the U.S. dairy industry to suppress the discovery in retail milk of live paraTB bacteria, a pathogen linked to type 1 diabetes.
-

Benefits of Turmeric Curcumin for Inflammatory Orbital Pseudotumor
From conjunctivitis to uveitis to a low-grade form of non-Hodgkin’s lymphoma, there is something in the spice turmeric with dramatic anti-inflammatory effects.
-

Does Bovine Insulin in Milk Trigger Type 1 Diabetes?
Is it the casein or the cow insulin that explains the link between milk consumption and the development of type I diabetes?
-

Does Casein in Milk Trigger Type 1 Diabetes?
Why might exposure to bovine proteins increase the risk of childhood-onset autoimmune type 1 diabetes?
-

Do Vitamin D Supplements Help with Diabetes, Weight Loss, and Blood Pressure?
Those with higher vitamin D levels tend to have lower rates of obesity, diabetes, and hypertension, but is it cause and effect? Interventional trials finally put vitamin D to the test.
-

Fighting Lupus with Turmeric: Good as Gold
A quarter teaspoon of the spice turmeric was put to the test for the treatment of uncontrollable lupus (SLE) nephritis in a randomized, double-blind, placebo-controlled clinical trial.
-

Anti-Inflammatory Diet for Depression
If depression can be induced with pro-inflammatory drugs, might an anti-inflammatory diet be effective in preventing and treating mood disorders?
-

Why Do Plant-Based Diets Help Rheumatoid Arthritis?
Rheumatoid arthritis may be triggered by autoimmune friendly fire against a urinary tract infection bacteria called Proteus mirabilis, which could help explain why sufferers randomized to a plant-based diet experience such remarkable benefit.
-

Lipotoxicity: How Saturated Fat Raises Blood Sugar
The reason those eating plant-based diets have less fat buildup in their muscle cells and less insulin resistance may be because saturated fats appear to impair blood sugar control the most.
-

Preventing Crohn’s Disease with Diet
Diets centered around whole plant foods may help prevent Crohn’s disease through the benefits of fiber on the maintenance of intestinal barrier function and the avoidance of certain processed food additives such as polysorbate 80.
-

How to Prevent Prediabetes in Children
Prediabetes is a disease in and of itself, associated with early damage to the eyes, kidneys, and heart. The explosion of diabetes in children is a result of our epidemic of childhood obesity. A plant-based diet may help, given that vegetarian kids grow up not only taller, but thinner.
-

How to Diagnose Gluten Intolerance
After a formal evaluation to rule out celiac disease, those who suspect they might have gluten sensitivity should first try improving their diet and then have other causes excluded before going on a gluten-free diet, since as many as 1 in 3 people who avoid gluten for symptom control end up having a different disease altogether.
-

Tick Bites, Meat Allergies, and Chronic Urticaria
The rising incidence of tick-bite induced meat allergies may account for cases of previously unexplained (“idiopathic”) persistent hives among children.
-

Alpha-Gal and the Lone Star Tick
Our immune response against a foreign molecule present in animal products may play a role in some allergic, autoimmune, and inflammatory disorders. This reaction is thought to underlie tick bite-triggered meat allergies.
-

Is Meat Glue Safe?
Used in about eight million pounds of meat every year in the United States, the “meat glue” enzyme, transglutaminase, has potential food safety and allergy implications.